Cvs Caremark Appeal Form Printable
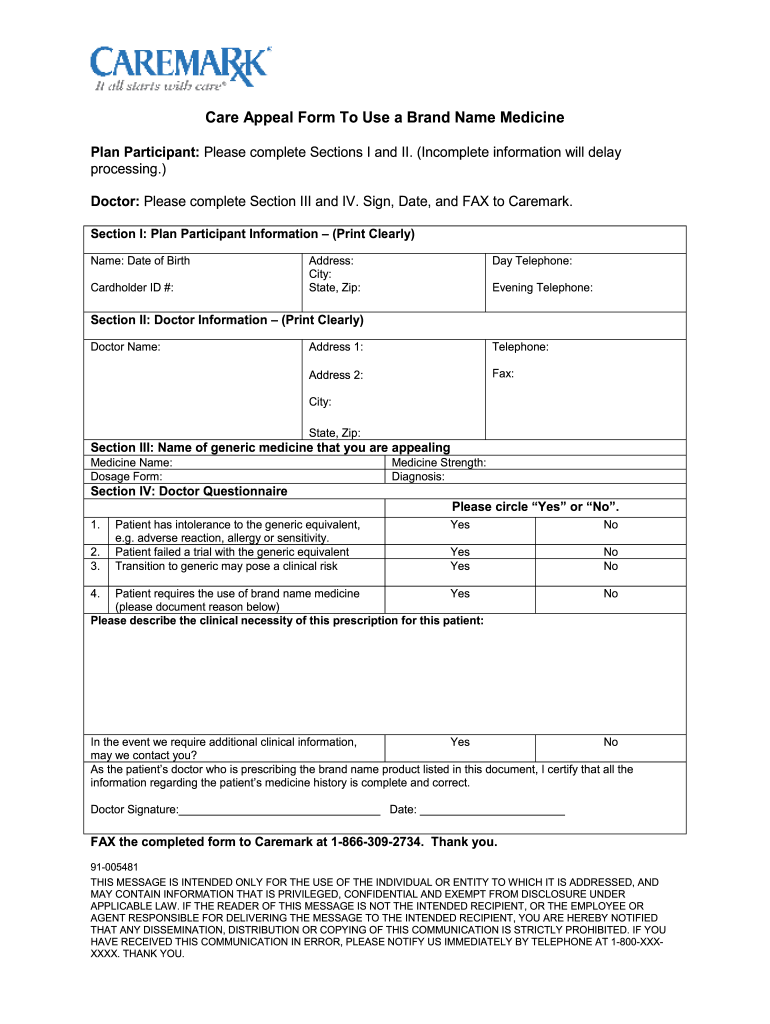
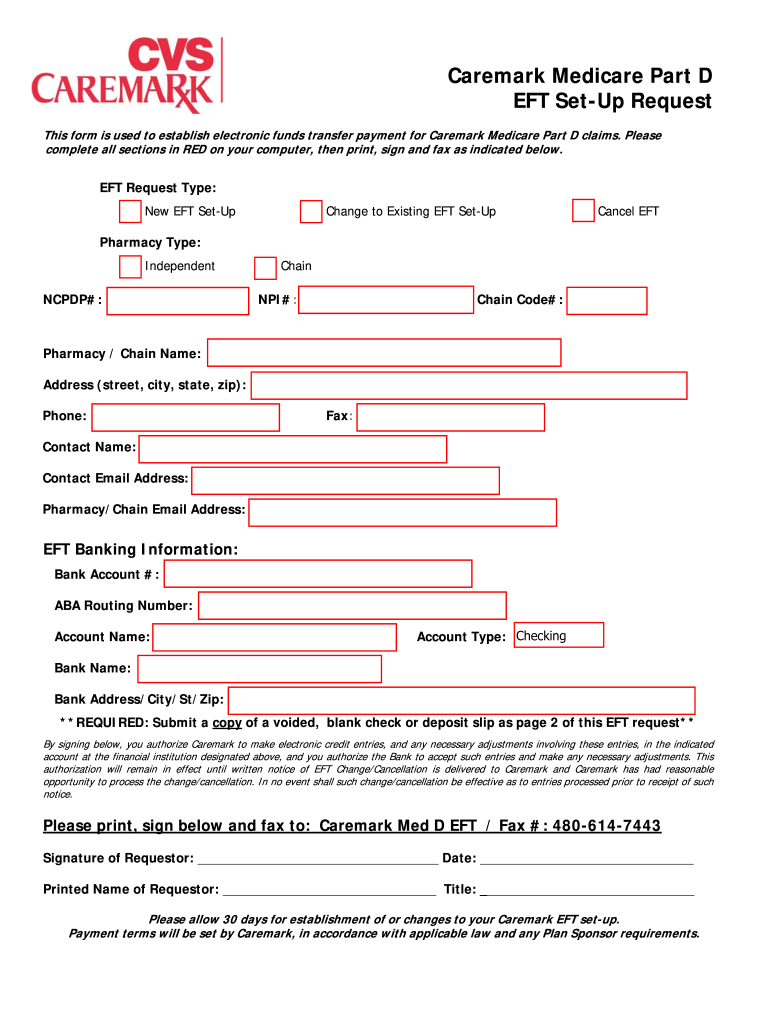
Cvs Caremark Appeal Form Printable - A pharmacist is available during normal business hours. Web learn how to appeal a denial of prior authorization for a prescription drug by cvs/caremark. All appeals are handled by cvs caremark, our pharmacy benefits manager. Mail service order form (english) formulario p/servicio por correo (español) Find out what information to include in your appeal and how to fax it to. The cvs caremark appeals department. Because we, silverscript employer pdp, denied your request for coverage of (or payment for) a. Web cvs caremark appeals dept. Web there are two types of appeals: An expedited appeal for urgent matters, and a standard appeal. Because we, silverscript employer pdp, denied your request for coverage of (or payment for) a. Cvs caremark customer care correspondence po box 6590 lee’s. Covermymeds automates the prior authorization (pa) process. Find out what information to include in your appeal and how to fax it to. Web there are two types of appeals: Web this form is available at: Because we, silverscript employer pdp, denied your request for coverage of (or payment for) a. For questions concerning your prescription (s), a pharmacist is available during normal business hours. Web troop excluded entity patient pay amount adjustment form; This information is provided in prior authorization denial letters and notifies members of their right to. The cvs caremark appeals department. A pharmacist is available during normal business hours. Web request for redetermination of medicare prescription drug denial. Web you have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. This information is provided in prior authorization denial letters and notifies members of their. Web learn how to appeal a denial of prior authorization for a prescription drug by cvs/caremark. Cvs caremark is dedicated to helping physicians manage and help their patients who are suffering from. Web step 2 submission requirements. Specialty pharmacy services, information and forms. Please provide as much information as. Web step 2 submission requirements. The cvs caremark appeals department. Specialty pharmacy services, information and forms. Web troop excluded entity patient pay amount adjustment form; Web request for redetermination of medicare prescription drug denial. Because we denied your request for coverage of (or payment for) a. Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. Web print plan forms download a form to start a new mail order prescription. Web you have 60 days from the date of our notice of denial of medicare prescription drug coverage. To get started, sign in or register for an account at caremark.com, or with. Web this form is available at: Cvs caremark is dedicated to helping physicians manage and help their patients who are suffering from. Web request for redetermination of medicare prescription drug denial. Mail service order form (english) formulario p/servicio por correo (español) This information is provided in prior authorization denial letters and notifies members of their right to appeal within 60 days of notice. Web there are two types of appeals: Web cvs caremark appeals dept. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Because we, silverscript employer pdp, denied your request for coverage of (or. All appeals are handled by cvs caremark, our pharmacy benefits manager. If you have other drugs you would like to request a. Web cvs caremark appeals dept. For questions concerning your prescription (s), a pharmacist is available during normal business hours. Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. Web step 2 submission requirements. This information is provided in prior authorization denial letters and notifies members of their right to appeal within 60 days of notice. Web print plan. Web you have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. The cvs caremark appeals department. To get started, sign in or register for an account at caremark.com, or with. Call the customer care number on your id card. This form may also be sent to us by mail or fax: The appeals operate in a similar fashion,. Because we denied your request for coverage of (or payment for) a. Web once an appeal is received, the appeal and all supporting documentation are reviewed and completed, including a notification to the member and physician, within the following. Mail service order form (english) formulario p/servicio por correo (español) Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. All appeals are handled by cvs caremark, our pharmacy benefits manager. Web troop excluded entity patient pay amount adjustment form; Web cvs caremark appeals dept. Web there are two types of appeals: Web covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web learn how to appeal a denial of prior authorization for a prescription drug by cvs/caremark.Caremark Appeal Form ≡ Fill Out Printable PDF Forms Online
Cvs Caremark Appeal PDF 20032024 Form Fill Out and Sign Printable
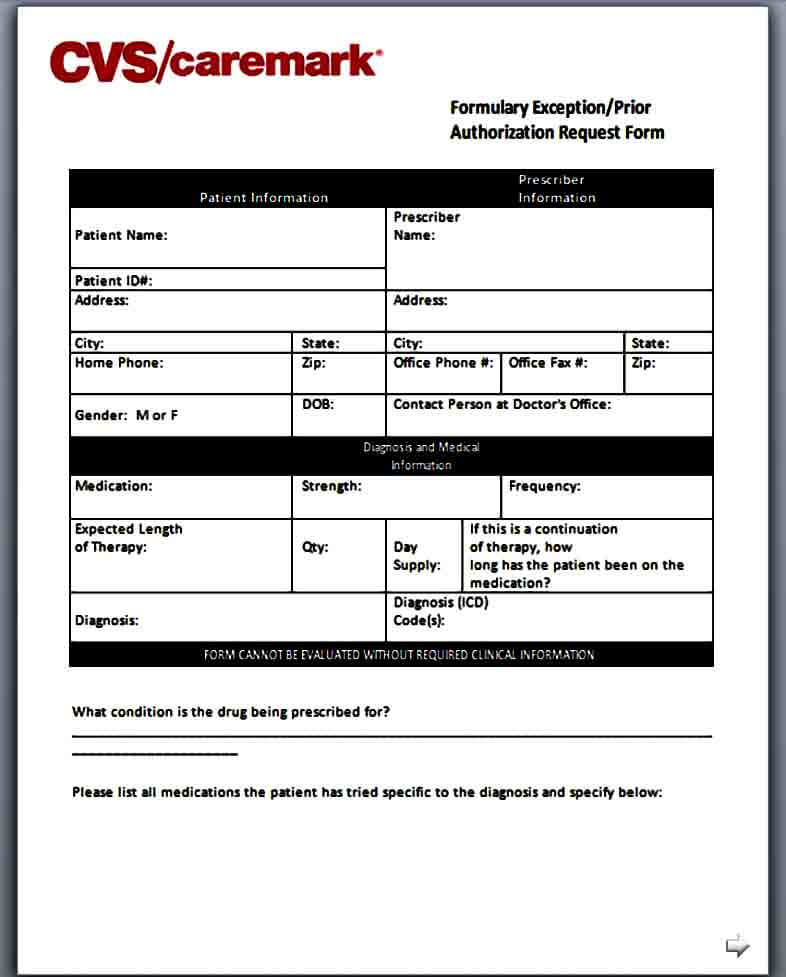
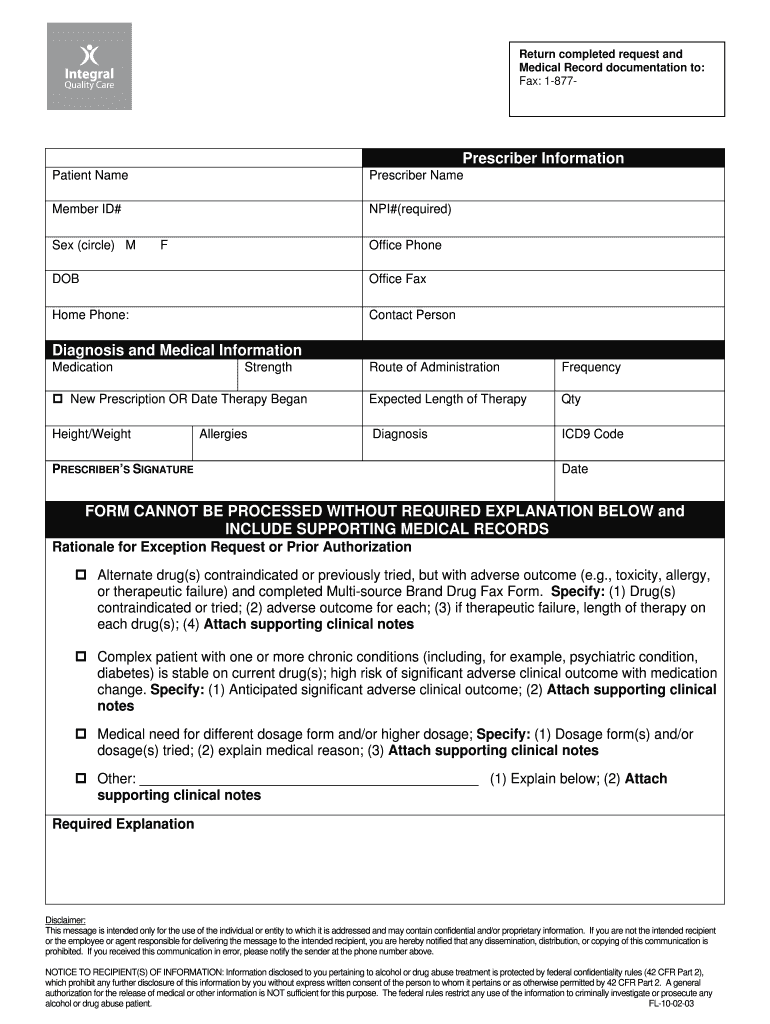
Template Caremark Prior Authorization Form Mous Syusa
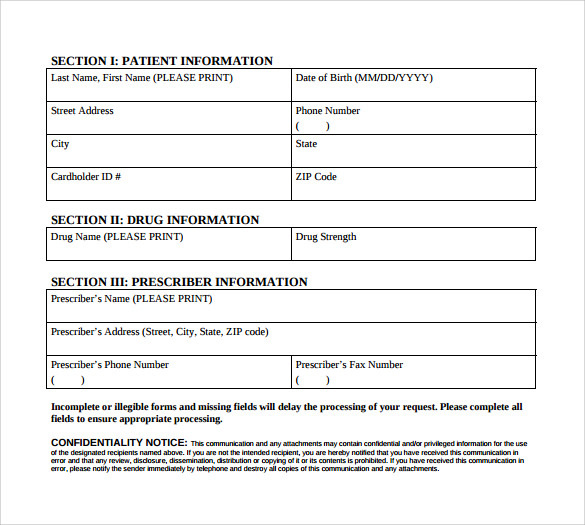
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF

Fill Free fillable Cvsprescriptclaimsform CVS Caremark Claim Form
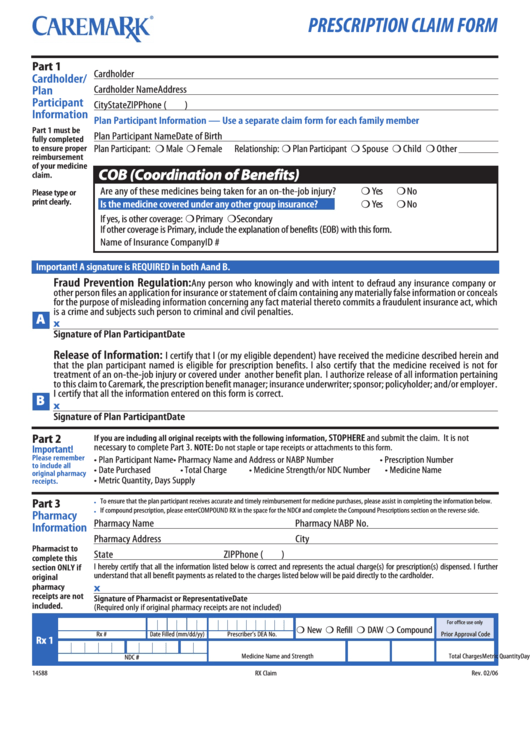
Top 20 Cvs Caremark Forms And Templates free to download in PDF format
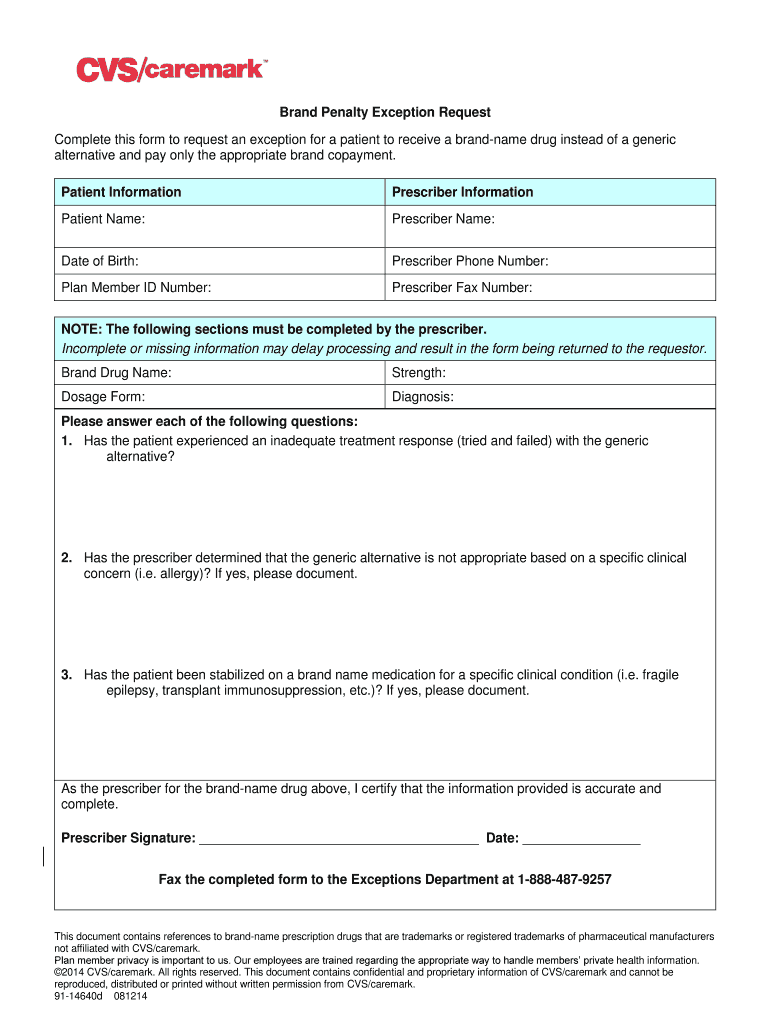
Caremark Brand Penalty Exception Form Fill Out and Sign Printable PDF
Cvs Caremark Appeal Form Edit & Share airSlate SignNow
Cvs caremark provider services Fill out & sign online DocHub
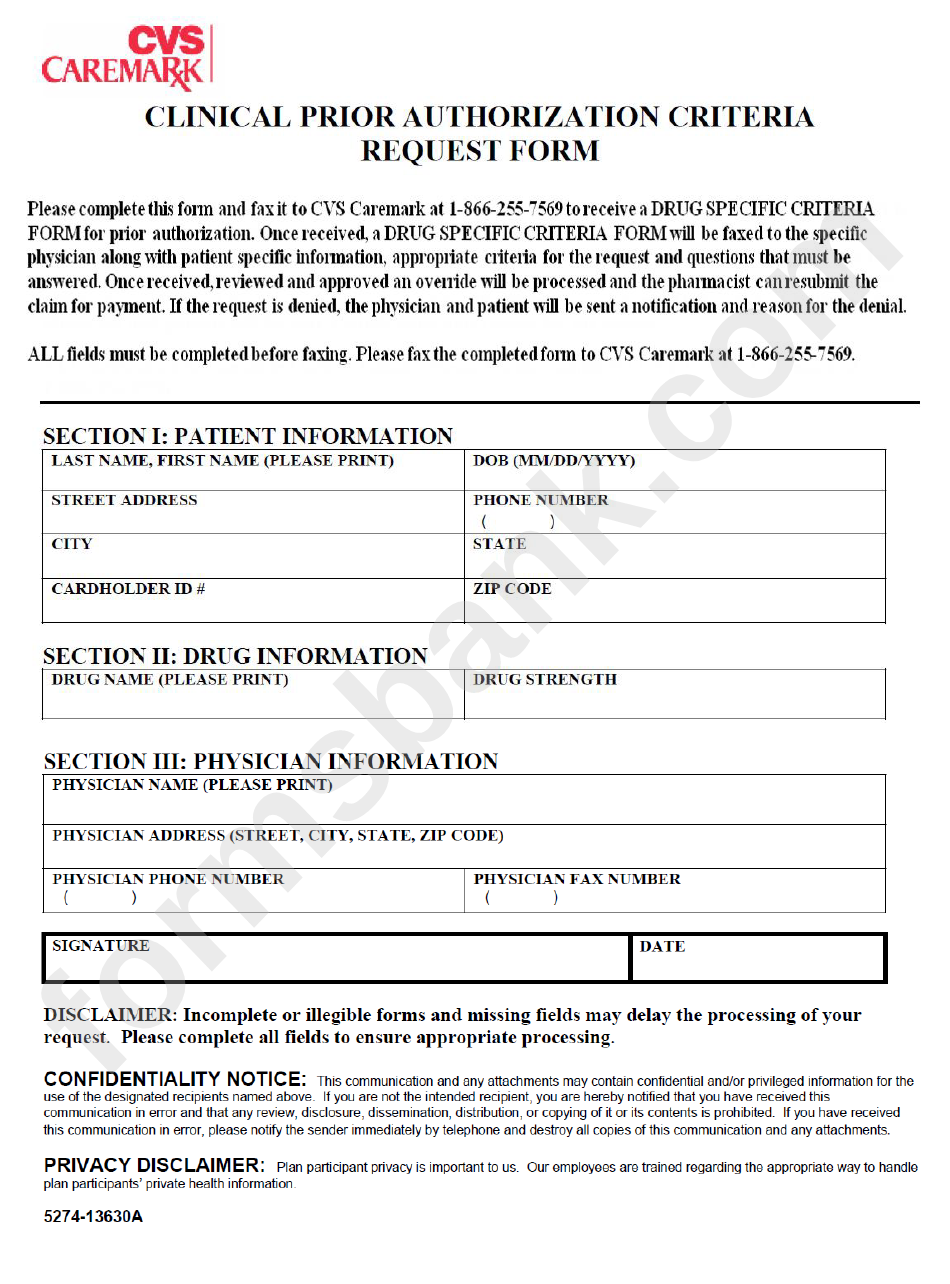
Caremark Prior Authorization Criteria Request Form printable pdf download
For Questions Concerning Your Prescription (S), A Pharmacist Is Available During Normal Business Hours.
Web Cvs Specialty Pharmacy Ncpdp Id 1466033 800 Biermann Court Mount Prospect, Il 60056.
If You Wish To Request A Medicare Part Determination (Prior Authorization Or Exception Request), Please See Your Plan’s Website.
This Information Is Provided In Prior Authorization Denial Letters And Notifies Members Of Their Right To Appeal Within 60 Days Of Notice.
Related Post: