Denial Management Process Flow Chart
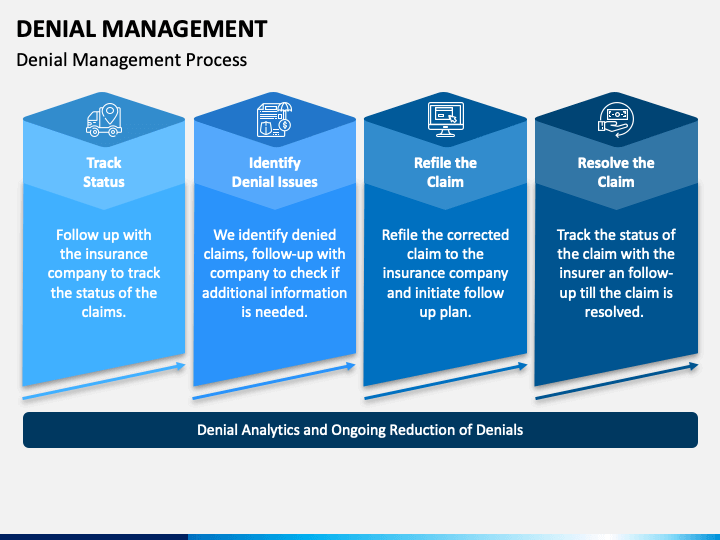
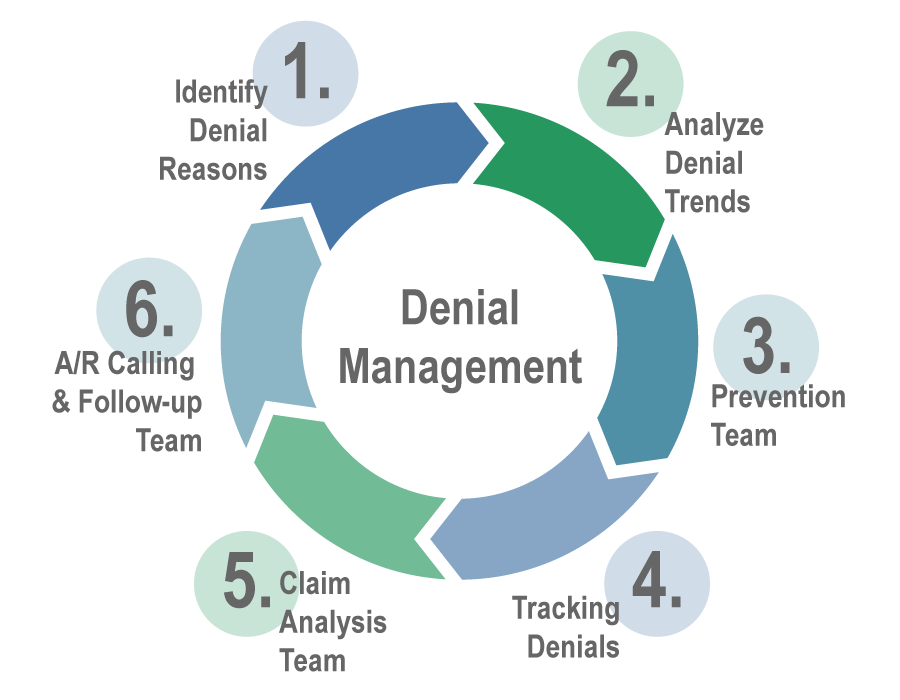
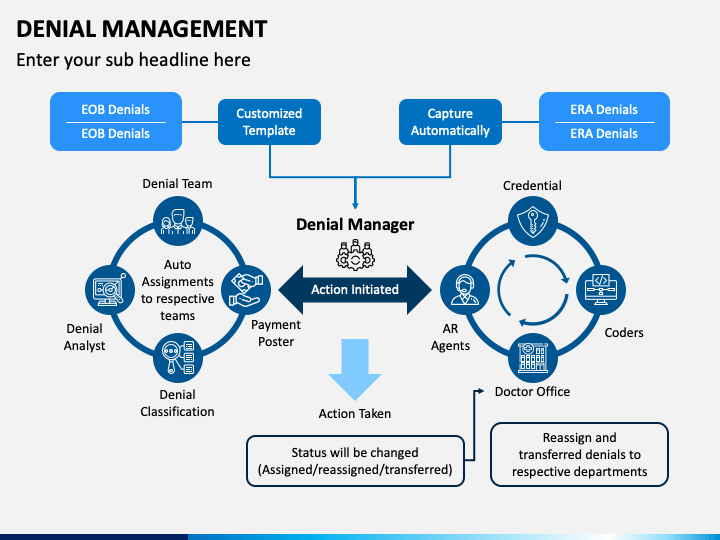
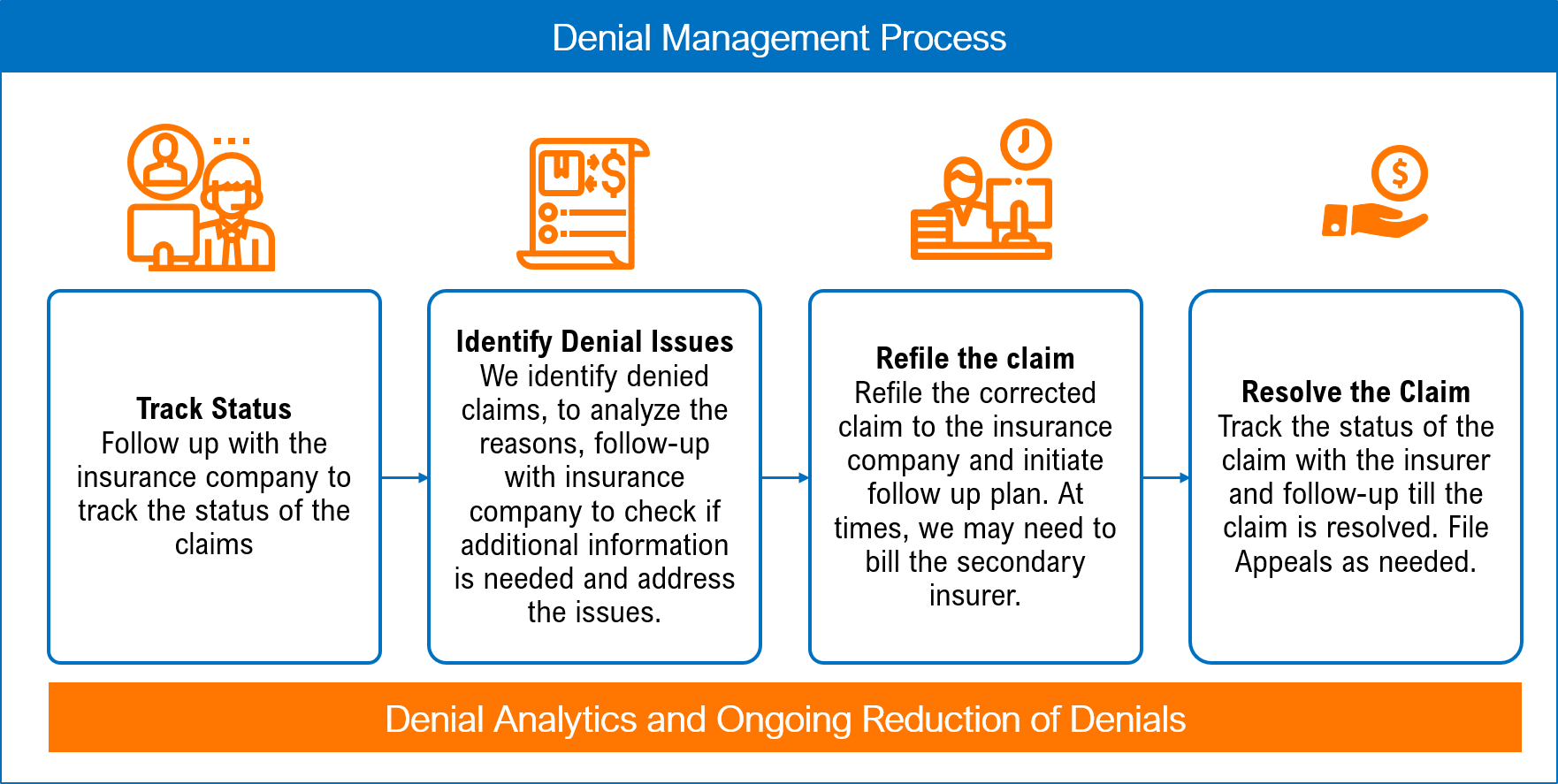
Denial Management Process Flow Chart - We have compiled a list of issues & actions in. Denial management is the process of dealing with insurance company denials at a hospital. Establish a denial management team. Web what is denial management? The purpose of this task is to minimize. Web track historical denials and payments. Every organization has a different claims. Web an effective program enables provider organizations to quickly correct rejected claims and maintain cash flow. Identify, manage, monitor and prevent. Web to determine a denials rate, hospitals should divide the total number of claims denied by the aggregate number of claims remitted for a select timeframe, the. Web learn how to navigate the complex terrain of claims denials efficiently with a denial management process flow chart. Web to determine a denials rate, hospitals should divide the total number of claims denied by the aggregate number of claims remitted for a select timeframe, the. What is not well known, however, is the important role. Every organization has a. Web what is denial management? Quantify and categorize denials by tracking, evaluating, and recording the trends. Denial management is the process of dealing with insurance company denials at a hospital. Web through effectively managing denials, facilities can: Zmake the registration process as easy as. Web through effectively managing denials, facilities can: Gather information about the claim, including the source (e.g., payer notification, claim status report), denial code, and reason for denial. Best practices and tips will help hospitals turn denials into. Web calculate a risk priority number (rpn) rpn = severity x occurrence x detection. Web the core steps of a denial management process. Highlights the areas were corrective actions can be. Web what is denial management? We have compiled a list of issues & actions in. Web learn how to navigate the complex terrain of claims denials efficiently with a denial management process flow chart. What is not well known, however, is the important role. Web learn how to navigate the complex terrain of claims denials efficiently with a denial management process flow chart. This tool serves as a roadmap for healthcare. Web track historical denials and payments. Web an effective program enables provider organizations to quickly correct rejected claims and maintain cash flow. We have compiled a list of issues & actions in. Web an effective program enables provider organizations to quickly correct rejected claims and maintain cash flow. Web through effectively managing denials, facilities can: What is not well known, however, is the important role. Web the core steps of a denial management process in healthcare include the following: Web what is denial management? Web track historical denials and payments. Review past claims and remit data to see when you’ve been paid correctly and when your claim was denied. Every organization has a different claims. Denial management is the process of dealing with insurance company denials at a hospital. We have compiled a list of issues & actions in. The purpose of this task is to minimize. Web the core steps of a denial management process in healthcare include the following: Web here are eight strategies for effective denial management in healthcare: We have compiled a list of issues & actions in. What is not well known, however, is the important role. Zmake the registration process as easy as. This tool serves as a roadmap for healthcare. Web the denials management training handbook is a clear, concise guide to the denials management process. Web the core steps of a denial management process in healthcare include the following: Web according to a recent advisory board survey, the median success rate for provider claim. This tool serves as a roadmap for healthcare. Denial management is the process of dealing with insurance company denials at a hospital. Web to determine a denials rate, hospitals should divide the total number of claims denied by the aggregate number of claims remitted for a select timeframe, the. Best practices and tips will help hospitals turn denials into. Web. Web the core steps of a denial management process in healthcare include the following: Highlights the areas were corrective actions can be. Establish a denial management team. Review past claims and remit data to see when you’ve been paid correctly and when your claim was denied. Quantify and categorize denials by tracking, evaluating, and recording the trends. Best practices and tips will help hospitals turn denials into. Web calculate a risk priority number (rpn) rpn = severity x occurrence x detection. Denial management is the process of dealing with insurance company denials at a hospital. Web according to a recent advisory board survey, the median success rate for provider claim denial appeals dropped from 56 percent to 45 percent for private heath. We have compiled a list of issues & actions in. Zmake the registration process as easy as. This tool serves as a roadmap for healthcare. Web in healthcare, denial management involves analyzing and preventing claim denials made by insurance companies or other relevant payers. Web to determine a denials rate, hospitals should divide the total number of claims denied by the aggregate number of claims remitted for a select timeframe, the. Web an effective program enables provider organizations to quickly correct rejected claims and maintain cash flow. Sort the fmea in descending order by rpn.
Denial Management Process Flow Chart

Denial Management Process Flow Chart
Denial Management Process Flow Chart
Denial Management Process Flow Chart
Denial Management Process Flow Chart
Denial Management Process Flow Chart

Denial Management Process Flow Chart

Denial Management Process Flow Chart

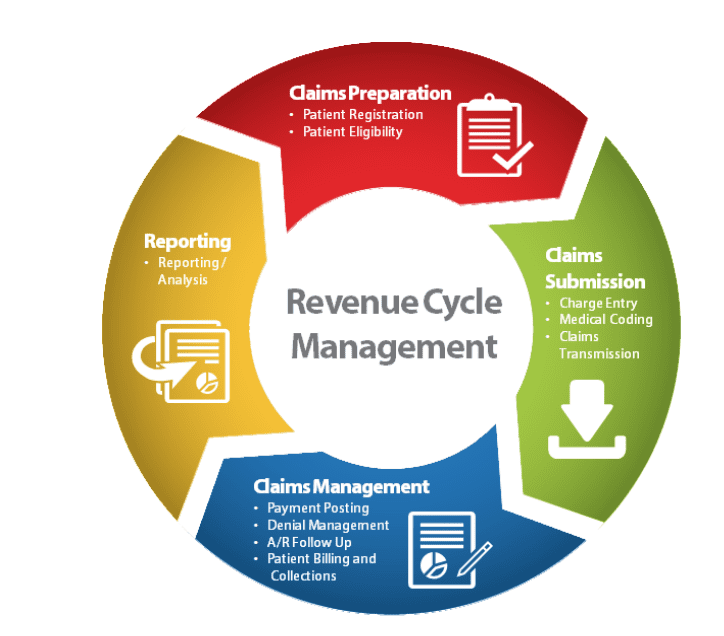
Denial Management Services in Medical Billing MedBillingExperts
Denial Management Process Flow Chart Labb by AG
The First Step In Effective Denial Management Is.
Here Are Some Facts About Denials:
Identify Shortcomings In Claim Submissions And Prevent Future Denials.
Identify, Manage, Monitor And Prevent.
Related Post: